Understanding Root Canal Treatment: Saving Your Natural Teeth
Root canal treatment, or endodontic therapy, is a specialized dental procedure aimed at eliminating infection, relieving tooth pain, and preserving the natural tooth structure. Contrary to common misconceptions, modern techniques have transformed this procedure into a comfortable and highly effective solution, boasting a success rate exceeding 95% PMC.
This comprehensive guide delves into every facet of endodontic therapy—from diagnosis to aftercare—empowering you to make informed decisions about your oral health.
The Science Behind Endodontic Therapy
Tooth Anatomy and Infection Pathways
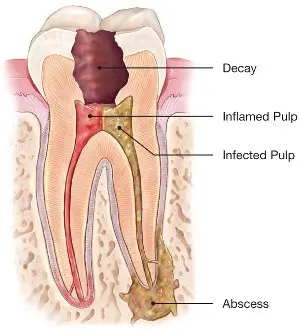
Understanding the internal structure of a tooth is crucial to grasp the importance of root canal treatment.
Pulp Chamber: Located at the center of the tooth, it houses nerves, blood vessels, and connective tissue.
Root Canals: Each tooth can have 1 to 4 canals, averaging 22mm in length, serving as pathways for nerves and blood vessels.
Infection Progression: Dental caries or trauma can allow bacteria to infiltrate the pulp, leading to inflammation (pulpitis) and, if untreated, necrosis.
Biological Objectives of Treatment
The primary goals of root canal therapy are:
Microbial Control: Eliminating 99.9% of pathogens within the canal system.
Space Preparation: Three-dimensional cleaning and shaping of canals to facilitate effective disinfection.
Sealing: Preventing recontamination by hermetically sealing the canal system.
Table: Endodontic Success Rates by Tooth Type
| Tooth Type | Success Rate | Special Considerations |
|---|---|---|
| Incisor | 98% | Typically straight canals |
| Premolar | 92% | Often have curved canals |
| Molar | 86% | Complex anatomy with multiple canals |
Advanced Diagnostic Techniques
Digital Imaging Revolution
Modern diagnostics have significantly enhanced the precision of endodontic therapy:
Cone Beam Computed Tomography (CBCT) provides 3D imaging with 0.076mm resolution, allowing detailed assessment of root canal morphology.
Electronic Apex Locators offer 94% accuracy in determining the working length of canals, minimizing the risk of over- or under-instrumentation.
Laser Fluorescence Caries Detection enhances the identification of carious lesions, ensuring comprehensive treatment planning.
Clinical Tests for Vitality Assessment
Assessing the health of the pulp tissue is vital:
Cold testing utilizes -50°C refrigerant spray to evaluate nerve response.
Electric Pulp Testing (EPT) offers 85% reliability in determining pulp vitality.
Selective anesthesia helps isolate the source of pain by numbing specific teeth or areas.
The Modern Root Canal Treatment Process
Step-by-Step Procedure
Access preparation involves creating a minimally invasive opening to reach the pulp chamber.
Shaping uses instruments with progressive taper (0.04 to 0.06) to clean and shape the canals.
Disinfection involves irrigating with 5.25% sodium hypochlorite (NaOCl) to eliminate bacteria and dissolve tissue remnants.
Obturation seals the canals using warm vertical compaction technique to prevent reinfection.
Technological Advancements
Rotary nickel-titanium files operate at 300 RPM with torque control, enhancing efficiency and reducing procedural errors.
Piezoelectric ultrasonics are effective in removing debris and calculus from intricate canal areas.
Bioceramic sealers exhibit 0.2% microleakage rates, promoting superior sealing and biocompatibility.
Specialized Endodontic Therapy Options
Microsurgical Endodontics
When conventional treatment isn’t sufficient, microsurgical approaches are employed:
Operating microscopes provide up to 20x magnification, enhancing visibility during procedures.
Ultrasonic retropreparation involves 3mm apical resection to remove infected tissue.
Mineral Trioxide Aggregate (MTA) retrofillings demonstrate a 92% success rate over five years.
Regenerative Endodontics
Aimed at revitalizing immature teeth with necrotic pulp:
Stem cells from apical papilla (SCAP) facilitate root development and healing.
Platelet-rich fibrin (PRF) acts as a scaffold, releasing growth factors to promote tissue regeneration.
Clinical outcomes: Studies have observed up to 48% increase in root length post-treatment.
Managing Tooth Pain Throughout Treatment
Anesthesia Protocols
Ensuring patient comfort is paramount:
Articaine offers 85% efficacy in anesthetizing mandibular molars.
Intraosseous injection systems deliver anesthesia directly into the bone for immediate effect.
Buffered lidocaine techniques enhance onset time and reduce injection discomfort.
Post-Treatment Comfort Measures
Occlusal reduction involves adjusting the bite to prevent undue pressure on the treated tooth.
Analgesic selection should tailor pain management strategies to individual patient needs.
Healing timeline: Most patients experience significant relief within 48–72 hours post-procedure.
Restoration After Root Canal Treatment
Coronal Seal Importance
A robust coronal restoration is critical:
Bacterial penetration risk is high—without proper sealing, bacteria can infiltrate within 24 hours.
Core buildup materials such as composite resins and amalgams show varying degrees of success.
Timing: Final restorations should ideally be placed within two weeks to prevent reinfection.
Prosthetic Considerations
The ferrule effect—a 2mm circumferential ferrule—enhances fracture resistance.
Material choices include monolithic zirconia for superior strength and lithium disilicate for better aesthetics.
Biomechanical load analysis ensures the restoration can withstand functional forces.
Endodontic Failures and Retreatment
Etiology of Failure
Understanding failure causes aids in effective retreatment:
Missed canals, such as MB2 canals present in 72% of maxillary molars, are often overlooked.
Fractures, especially vertical root fractures, can compromise tooth integrity.
Microleakage due to poor sealing allows bacterial infiltration, leading to reinfection.
Advanced Retreatment Techniques
Gutta-percha removal systems utilize rotary, manual, or ultrasonic instruments, sometimes with solvents, to clear previous fillings.
Calcium hydroxide dressings serve as intracanal medicaments to eliminate residual bacteria.
Decision algorithms help determine whether retreatment or extraction followed by implant placement is more appropriate.
The Future of Endodontic Therapy
Bioceramic Innovations
Advancements in materials science are shaping the future:
Bioactive dentin replacement materials mimic natural dentin properties.
Antimicrobial sealers incorporate agents to continuously combat infection.

